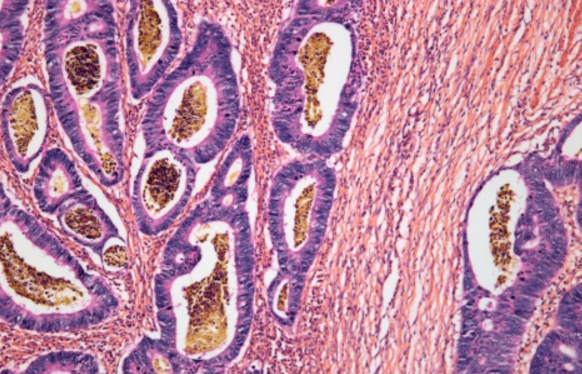
Inflammatory bowel disease (IBD) involves chronic inflammation of all or part of the digestive system. Generally speaking, IBD includes ulcerative colitis and Crohn’s disease. The most common age of onset is between 20-40 years old; however, new onsets of the disease can be seen in children and elderly as well. Etiology of IBD is multi-factorial, environmental factors, genetics, infections and immune system intertwined leading to the immune system erroneously attacking the patient’s own digestive system. Symptoms of ulcerative colitis and Crohn’s disease are very similar. Patient may suffer from tummy pain, diarrhea, blood mixed with stool, and weight loss due to decreased appetite and malabsorption. Besides symptoms of the digestive system, patients may also have inflammations in the joints, eyes, skin and bile ducts.
Ulcerative colitis mainly affects the colon and rectum, and causing inflammation at the innermost lining of the colon and rectum. Crohn’s disease, on the other hand, may affect anywhere of the digestive tract from the oral cavity down to the anus, and causing inflammation across all the layers of the digestive tract from the inside to the outside, sometimes affecting nearby organs. There is no definitive test to differentiate the 2 diseases. Gastroenterologist need to gather clinical information, blood tests, endoscopic findings and histology results in order to make a diagnosis. Tuberculosis infection of the digestive tract may present similar to Crohn’s disease, so extra care is needed to rule out infection before starting treatment.
Treatment strategy of IBD involves suppression of immune system with steroids and/or other immunosuppressive medications. Recent development of biologics allows control of more severe or refractory diseases. For uncontrollable ulcerative colitis, surgical removal of the whole large bowel is essentially a cure. The role of surgery in Crohn’s disease is to alleviate complications such as bowel obstruction, perforation of bowel wall and abnormal tracts connecting the gut to adjacent organs. IBD must be persistently and effectively controlled to avoid or minimize life-threatening complications and colonic cancers.
發炎性腸病
發炎性腸病(炎症性腸病)一般而言包括兩種疾病:潰瘍性腸炎及克隆氏症。這兩種慢性腸道疾病的發生原因可能與環境因素,基因,感染和免疫系統的互相作用有關,導致身體的免疫系統錯誤地攻擊腸道。最常見發病的歲數為20至40歲,但也可能在兒童和老人家發病。兩種病的症狀非常近似,包括腹痛、腹瀉和大便有血、因為胃口欠佳和營養吸收功能受捐導致病人體重會持續下降。除消化系統外,其他相關症狀包括關節炎、壞疽性膿皮症、眼色素層炎及硬化性膽管炎。
潰瘍性腸炎一般只影響大腸,而且只是腸道內的表層黏膜發炎。克隆氏症則可影響腸胃道內從口腔至肛門的任何部分,而發炎可由腸道內層至腸道外層及影響附近的器官。現在沒有特定方法將兩種病距分,醫生要根據臨床診斷,血液化驗結果,內視鏡檢查和抽取腸壁組織檢查來幫助診症。有些克隆氏症病人的病症跟腸結核非常相似,一定要小心排除後者才能確診。
發炎性腸病的治療需要長期服藥來壓抑炎症,如類固醇及其他抑制免疫系統藥物。近年開始使用的生物製劑可改善較嚴重的病情。病情最嚴重的潰瘍性腸炎病人可選擇將大腸切除而得到控制。克隆氏症患者可能出現併發症如腸道因腫脹而做成阻塞,腸道穿破或黏連至其他器官,需要外科手術治療。發炎性腸病病情必須長期受控,否則會有機會出現致命的併發症或大腸癌。
Image Source: Healthline